Final Summary, 48 Hours
March/05/2011 09:44 AM
I am picking up from friday morning...
After breaking away from OR: go to see Basiwell’s mom in ER to work on her newly operated hand. After the morning, it felt nice to just do PT and especially for someone whose son has been so kind and helpful. Remember, patients are given virtually no pain meds. She endures the necessary early range of motion and even with increased pain, she is grateful for my time and efforts.
Go back to house and change scrubs. Return to OR to see if any help is needed.
Patient 1: O2 sats drop every time he is taken off O2. Have I mentioned they have a shortage of O2 and during his morning surgery, we ran out of O2? (this is not the first time during the week that they have run out if O2). His saturation dropped to 16.
Suddenly Sheila arrives with an O2 tank and we are back up and running. Ruben has ruled out various causes for poor O2. Most probably, a pneumothorax. Problem... no available chest tube kit and no one who feels well rehearsed in placing chest tube. General surgeon from Port-au-Prince on his way... It will take 5 hours.
There are more patients who need attention in OR so we need to devise a method to get this patient on to a portable O2. There is one unit with a nasal cannula – Not going to be enough. Ruben and I jerry-rig a face mask with Ambu Bag to patient and unit. Patient brought to recovery.
A word about recovery...
Recovery is a room with NO monitoring equipment. The team has brought three O2 pulseoximeters with us - thank you Ruben. During this process, patients 2 & 3 have been cared for as well.
Ok...so it is 3:30pm now (I regressed a bit) and the one inpatient boy I really wanted to work with (soccer injury), just so happens to wheel himself over to "clinic/PT". I actually had time to work with him and emphasize the importance of working on his own. It will be at least 4 weeks before another PT will be here.
The therapy team meets back on ward to finish up treatment plans, visit with newborn (who I swaddled and gave his first bottle). Mom still unresponsive. We find dad a CHAIR so he can sit down in room. He has not named baby and asks if I would like to name baby. I choose David. They pronounce it Dah-veed, like it is Hebrew.
Also stop by and meet newborn healthy twins with healthy mom. She delivered one day ago. Another teammate was asked to name the twins.
In front of ward there is a courtyard with an unused grassy area. Several team members and translators start up a game of frisbee. It is the first time during the work week where any of us have played around. We attract attention from all of the patients who we have been trying to get outside all week (with great success). Since most of them have some variety of damaged lower extremities, I suggest to the group that we try a “wheel barrel race” and have them race across field while we support their legs (good upper body strengthening!). At first the patients looked at us like we were insane but we talked two into it. Well, this drew just about every staff member and patient out to courtyard to watch. Two of us helped this one patient with a huge fixator devise on his leg. Little did we know that he had a competitive spirit and "walked" so fast on hands, his fixator device practically pierced through my thigh. It was a tie.
So much excitement. Everyone laughing and cheering. More want to race... so this was clearly a highlight of the week as my initial goal was to get everyone outside and create a healthy environment. Said goodbyes to patients and translators after race.
Home for last dinner. Surgeons still in OR. We all head back up to hospital to inquire on surgery cases and recovery room patients. The general surgeon has arrived and the patient with the acute peritonitis (not so acute at this point and surprisingly alive) will finally have his surgery. This is the guy Ruben was running for pain medicine last night when pregnant women showed up. After this surgery patient 1 will get his chest tube. He does not look good. Several team members bring father/husband something to eat. I cannot go back to this room as it is far too emotional for me.
I stop by ER to write/send my initial 48 hour blog (only place with WiFi). Can't write it all at once; too tired and drained.
Final evening, we all debrief about the week and discuss highlights and hard moments. We laugh about some of the crazy stuff that gas happened through out the week. Most of week we had no electricity at house. Hospital operated off generator and would shut down at 10 pm. But lucky for us, we have had electricity since 3:00pm. It is now 1:30 am and I still need to take a cold shower and be up for airport ride at 4:15am... so no sleep for me.
This morning we pack up van, load luggage on top and head out for local airport (75 minutes down the mountain). We are flying to Port-au-Prince as we "weigh a lot less" having unloaded all of our donated goods and can get on a small plane. On way to airport, Sheila gets call from Rudy, the Haitian MD who is in charge (his regular workday schedule is 7:30 am where he leads prayer service to 10:00 pm) I have never seen a doctor work harder with such restricted conditions and manage to still make lots of joked. He has been up all night (second night in a row) and tells Sheila that patient 1 has died and another is being taken back to OR. So much in one week and of course only the tiniest dent on the need in Haiti.
At airport finishing this, looking forward to my husband being at airport and a long HOT shower.
Hard to think about returning to the chaos of our everyday lives. So much to do!!
After breaking away from OR: go to see Basiwell’s mom in ER to work on her newly operated hand. After the morning, it felt nice to just do PT and especially for someone whose son has been so kind and helpful. Remember, patients are given virtually no pain meds. She endures the necessary early range of motion and even with increased pain, she is grateful for my time and efforts.
Go back to house and change scrubs. Return to OR to see if any help is needed.
Patient 1: O2 sats drop every time he is taken off O2. Have I mentioned they have a shortage of O2 and during his morning surgery, we ran out of O2? (this is not the first time during the week that they have run out if O2). His saturation dropped to 16.
Suddenly Sheila arrives with an O2 tank and we are back up and running. Ruben has ruled out various causes for poor O2. Most probably, a pneumothorax. Problem... no available chest tube kit and no one who feels well rehearsed in placing chest tube. General surgeon from Port-au-Prince on his way... It will take 5 hours.
There are more patients who need attention in OR so we need to devise a method to get this patient on to a portable O2. There is one unit with a nasal cannula – Not going to be enough. Ruben and I jerry-rig a face mask with Ambu Bag to patient and unit. Patient brought to recovery.
A word about recovery...
Recovery is a room with NO monitoring equipment. The team has brought three O2 pulseoximeters with us - thank you Ruben. During this process, patients 2 & 3 have been cared for as well.
Ok...so it is 3:30pm now (I regressed a bit) and the one inpatient boy I really wanted to work with (soccer injury), just so happens to wheel himself over to "clinic/PT". I actually had time to work with him and emphasize the importance of working on his own. It will be at least 4 weeks before another PT will be here.
The therapy team meets back on ward to finish up treatment plans, visit with newborn (who I swaddled and gave his first bottle). Mom still unresponsive. We find dad a CHAIR so he can sit down in room. He has not named baby and asks if I would like to name baby. I choose David. They pronounce it Dah-veed, like it is Hebrew.
Also stop by and meet newborn healthy twins with healthy mom. She delivered one day ago. Another teammate was asked to name the twins.
In front of ward there is a courtyard with an unused grassy area. Several team members and translators start up a game of frisbee. It is the first time during the work week where any of us have played around. We attract attention from all of the patients who we have been trying to get outside all week (with great success). Since most of them have some variety of damaged lower extremities, I suggest to the group that we try a “wheel barrel race” and have them race across field while we support their legs (good upper body strengthening!). At first the patients looked at us like we were insane but we talked two into it. Well, this drew just about every staff member and patient out to courtyard to watch. Two of us helped this one patient with a huge fixator devise on his leg. Little did we know that he had a competitive spirit and "walked" so fast on hands, his fixator device practically pierced through my thigh. It was a tie.
So much excitement. Everyone laughing and cheering. More want to race... so this was clearly a highlight of the week as my initial goal was to get everyone outside and create a healthy environment. Said goodbyes to patients and translators after race.
Home for last dinner. Surgeons still in OR. We all head back up to hospital to inquire on surgery cases and recovery room patients. The general surgeon has arrived and the patient with the acute peritonitis (not so acute at this point and surprisingly alive) will finally have his surgery. This is the guy Ruben was running for pain medicine last night when pregnant women showed up. After this surgery patient 1 will get his chest tube. He does not look good. Several team members bring father/husband something to eat. I cannot go back to this room as it is far too emotional for me.
I stop by ER to write/send my initial 48 hour blog (only place with WiFi). Can't write it all at once; too tired and drained.
Final evening, we all debrief about the week and discuss highlights and hard moments. We laugh about some of the crazy stuff that gas happened through out the week. Most of week we had no electricity at house. Hospital operated off generator and would shut down at 10 pm. But lucky for us, we have had electricity since 3:00pm. It is now 1:30 am and I still need to take a cold shower and be up for airport ride at 4:15am... so no sleep for me.
This morning we pack up van, load luggage on top and head out for local airport (75 minutes down the mountain). We are flying to Port-au-Prince as we "weigh a lot less" having unloaded all of our donated goods and can get on a small plane. On way to airport, Sheila gets call from Rudy, the Haitian MD who is in charge (his regular workday schedule is 7:30 am where he leads prayer service to 10:00 pm) I have never seen a doctor work harder with such restricted conditions and manage to still make lots of joked. He has been up all night (second night in a row) and tells Sheila that patient 1 has died and another is being taken back to OR. So much in one week and of course only the tiniest dent on the need in Haiti.
At airport finishing this, looking forward to my husband being at airport and a long HOT shower.
Hard to think about returning to the chaos of our everyday lives. So much to do!!
0 Comments
Last 48 hours: Part Two
March/04/2011 05:48 PM
Friday AM Prayer service
They sing Hatikva in Creole...????
8:00 am: Head to ward.
Baby doing OK.
Mom: no urine output, HTN, heart rate 145. Unconscious
Husband overwhelmed...No one has explained what is going on to dad.
Dealing with mom...when...
Our orthopedic surgeon, Noah, comes to get us...
3 Trauma patients arrived in “ER”:
All morning until 2:30 running around ER and OR. Suddenly I’m a trauma nurse!
There is so much more but I need to go back to house to pack.
I don't think I will ever be the same after this week...
They sing Hatikva in Creole...????
8:00 am: Head to ward.
Baby doing OK.
Mom: no urine output, HTN, heart rate 145. Unconscious
Husband overwhelmed...No one has explained what is going on to dad.
Dealing with mom...when...
Our orthopedic surgeon, Noah, comes to get us...
3 Trauma patients arrived in “ER”:
- Pt. 1: Eyeball out, fractured orbit, head injury, patella fracture, tibia laceration, agitated.
- Pt. 2: Face laceration, huge tibia deep wound, probable head injury
- Pt. 3: Open thigh wound, in shock,
All morning until 2:30 running around ER and OR. Suddenly I’m a trauma nurse!
There is so much more but I need to go back to house to pack.
I don't think I will ever be the same after this week...
Last 48 hours: Part One
March/03/2011 08:00 PM
Thursday night: 8:00 pm rounds in ER
-- Patient with acute peritonitis. No general surgeon.
We leave for ward; our anesthesiologist goes to pharmacy for pain meds.
On ward rounding...
Anesthesiologist comes back — Emergency! Need all of you at ER.
Pregnant woman with eclampsia, seizure at clinic; transferred 2.5 hrs in a FLATBED truck to ER.
She is placed on mat on ground in front of ER, hemorrhaging.
Baby born on mat; mom in distress.
Grab baby with placenta wrapped in someone’s jacket.
Take baby to room; cord cut. No formula. No infant attire
Mom in acute distress, bleeding. O2 65, hypertension 180/130, heart rate 155
Father in shock
Baby; formula; no hot water... also no electricity!
Teammate to guest house; heat water
No GYN, no general surgeon.
Our team stays with pts until 12:30am
Baby fine, but Mom in coma
Dad standing: use a half clean sheet on empty bed for Dad to rest
(patients have to bring all linens, food, etc. - family not prepared)
-- Patient with acute peritonitis. No general surgeon.
We leave for ward; our anesthesiologist goes to pharmacy for pain meds.
On ward rounding...
Anesthesiologist comes back — Emergency! Need all of you at ER.
Pregnant woman with eclampsia, seizure at clinic; transferred 2.5 hrs in a FLATBED truck to ER.
She is placed on mat on ground in front of ER, hemorrhaging.
Baby born on mat; mom in distress.
Grab baby with placenta wrapped in someone’s jacket.
Take baby to room; cord cut. No formula. No infant attire
Mom in acute distress, bleeding. O2 65, hypertension 180/130, heart rate 155
Father in shock
Baby; formula; no hot water... also no electricity!
Teammate to guest house; heat water
No GYN, no general surgeon.
Our team stays with pts until 12:30am
Baby fine, but Mom in coma
Dad standing: use a half clean sheet on empty bed for Dad to rest
(patients have to bring all linens, food, etc. - family not prepared)
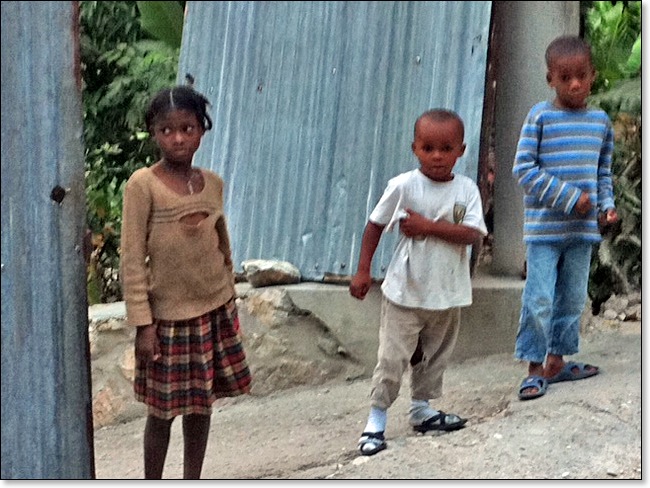
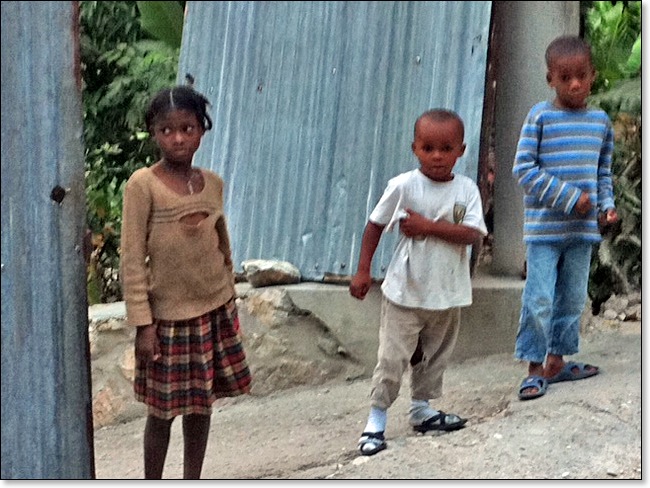
Children who live nearby
March/03/2011 09:33 AM
These children were very excited to see us pass by their home.
Click to view photo location in Google Maps
Click to view photo location in Google Maps
Family leaving funeral
March/02/2011 07:09 PM
A 30-year employee of the hospital died on Monday. The hospital "closed down" this afternoon so staff could attend funeral. I had 2 clinic patients so I missed the service. Funerals are a big deal here. Did catch some good photos after and video.

Click to view photo location in Google Maps
After funeral, 2 guys from hospital took Noah, Ruben, Max and I on a hike to their homes. At Basiwell's home they grow and roast coffee. He wanted us to see his moms hand; carpal tunnel surgery 5 years ago with full hand contracture from not moving it. She may have surgery tomorrow.
On to Jimmy's house. He makes honey and showed us his honeybees. Then he let us taste his honey -- truly fantastic!
The hike provided a real look in to the way the locals live. They have a higher quality of life than Port-au-Prince.
Evening rounds tonight from 7-9:30. Five surgeries scheduled tomorrow; more ortho follow-ups for clinic and 40-50 inpatients who need PT.

Click to view photo location in Google Maps
After funeral, 2 guys from hospital took Noah, Ruben, Max and I on a hike to their homes. At Basiwell's home they grow and roast coffee. He wanted us to see his moms hand; carpal tunnel surgery 5 years ago with full hand contracture from not moving it. She may have surgery tomorrow.
On to Jimmy's house. He makes honey and showed us his honeybees. Then he let us taste his honey -- truly fantastic!
The hike provided a real look in to the way the locals live. They have a higher quality of life than Port-au-Prince.
Evening rounds tonight from 7-9:30. Five surgeries scheduled tomorrow; more ortho follow-ups for clinic and 40-50 inpatients who need PT.
"Haiti Medical Trip February-March 2011"
March/02/2011 06:58 PM
Here is a link to a blog written by the group leader. He is a very kind, helpful and caring man.
http://msreinhard.blogspot.com/
http://msreinhard.blogspot.com/
Little girl/beanie baby
March/01/2011 07:11 AM
Bad picture. The good ones are on regular camera.
This girl's legs were crushed in the earthquake. She has a below knee amp. On right. Her left tibia/fibula have slowly healing fractures. She has a prosthesis for her right which has become the "good leg".
She was sad and serious until I gave her the beanie!!! I am SO glad I brought them.

Click to view photo location in Google Maps
This girl's legs were crushed in the earthquake. She has a below knee amp. On right. Her left tibia/fibula have slowly healing fractures. She has a prosthesis for her right which has become the "good leg".
She was sad and serious until I gave her the beanie!!! I am SO glad I brought them.

Click to view photo location in Google Maps

