Final Summary, 48 Hours
March/05/2011 09:44 AM
I am picking up from friday morning...
After breaking away from OR: go to see Basiwell’s mom in ER to work on her newly operated hand. After the morning, it felt nice to just do PT and especially for someone whose son has been so kind and helpful. Remember, patients are given virtually no pain meds. She endures the necessary early range of motion and even with increased pain, she is grateful for my time and efforts.
Go back to house and change scrubs. Return to OR to see if any help is needed.
Patient 1: O2 sats drop every time he is taken off O2. Have I mentioned they have a shortage of O2 and during his morning surgery, we ran out of O2? (this is not the first time during the week that they have run out if O2). His saturation dropped to 16.
Suddenly Sheila arrives with an O2 tank and we are back up and running. Ruben has ruled out various causes for poor O2. Most probably, a pneumothorax. Problem... no available chest tube kit and no one who feels well rehearsed in placing chest tube. General surgeon from Port-au-Prince on his way... It will take 5 hours.
There are more patients who need attention in OR so we need to devise a method to get this patient on to a portable O2. There is one unit with a nasal cannula – Not going to be enough. Ruben and I jerry-rig a face mask with Ambu Bag to patient and unit. Patient brought to recovery.
A word about recovery...
Recovery is a room with NO monitoring equipment. The team has brought three O2 pulseoximeters with us - thank you Ruben. During this process, patients 2 & 3 have been cared for as well.
Ok...so it is 3:30pm now (I regressed a bit) and the one inpatient boy I really wanted to work with (soccer injury), just so happens to wheel himself over to "clinic/PT". I actually had time to work with him and emphasize the importance of working on his own. It will be at least 4 weeks before another PT will be here.
The therapy team meets back on ward to finish up treatment plans, visit with newborn (who I swaddled and gave his first bottle). Mom still unresponsive. We find dad a CHAIR so he can sit down in room. He has not named baby and asks if I would like to name baby. I choose David. They pronounce it Dah-veed, like it is Hebrew.
Also stop by and meet newborn healthy twins with healthy mom. She delivered one day ago. Another teammate was asked to name the twins.
In front of ward there is a courtyard with an unused grassy area. Several team members and translators start up a game of frisbee. It is the first time during the work week where any of us have played around. We attract attention from all of the patients who we have been trying to get outside all week (with great success). Since most of them have some variety of damaged lower extremities, I suggest to the group that we try a “wheel barrel race” and have them race across field while we support their legs (good upper body strengthening!). At first the patients looked at us like we were insane but we talked two into it. Well, this drew just about every staff member and patient out to courtyard to watch. Two of us helped this one patient with a huge fixator devise on his leg. Little did we know that he had a competitive spirit and "walked" so fast on hands, his fixator device practically pierced through my thigh. It was a tie.
So much excitement. Everyone laughing and cheering. More want to race... so this was clearly a highlight of the week as my initial goal was to get everyone outside and create a healthy environment. Said goodbyes to patients and translators after race.
Home for last dinner. Surgeons still in OR. We all head back up to hospital to inquire on surgery cases and recovery room patients. The general surgeon has arrived and the patient with the acute peritonitis (not so acute at this point and surprisingly alive) will finally have his surgery. This is the guy Ruben was running for pain medicine last night when pregnant women showed up. After this surgery patient 1 will get his chest tube. He does not look good. Several team members bring father/husband something to eat. I cannot go back to this room as it is far too emotional for me.
I stop by ER to write/send my initial 48 hour blog (only place with WiFi). Can't write it all at once; too tired and drained.
Final evening, we all debrief about the week and discuss highlights and hard moments. We laugh about some of the crazy stuff that gas happened through out the week. Most of week we had no electricity at house. Hospital operated off generator and would shut down at 10 pm. But lucky for us, we have had electricity since 3:00pm. It is now 1:30 am and I still need to take a cold shower and be up for airport ride at 4:15am... so no sleep for me.
This morning we pack up van, load luggage on top and head out for local airport (75 minutes down the mountain). We are flying to Port-au-Prince as we "weigh a lot less" having unloaded all of our donated goods and can get on a small plane. On way to airport, Sheila gets call from Rudy, the Haitian MD who is in charge (his regular workday schedule is 7:30 am where he leads prayer service to 10:00 pm) I have never seen a doctor work harder with such restricted conditions and manage to still make lots of joked. He has been up all night (second night in a row) and tells Sheila that patient 1 has died and another is being taken back to OR. So much in one week and of course only the tiniest dent on the need in Haiti.
At airport finishing this, looking forward to my husband being at airport and a long HOT shower.
Hard to think about returning to the chaos of our everyday lives. So much to do!!
After breaking away from OR: go to see Basiwell’s mom in ER to work on her newly operated hand. After the morning, it felt nice to just do PT and especially for someone whose son has been so kind and helpful. Remember, patients are given virtually no pain meds. She endures the necessary early range of motion and even with increased pain, she is grateful for my time and efforts.
Go back to house and change scrubs. Return to OR to see if any help is needed.
Patient 1: O2 sats drop every time he is taken off O2. Have I mentioned they have a shortage of O2 and during his morning surgery, we ran out of O2? (this is not the first time during the week that they have run out if O2). His saturation dropped to 16.
Suddenly Sheila arrives with an O2 tank and we are back up and running. Ruben has ruled out various causes for poor O2. Most probably, a pneumothorax. Problem... no available chest tube kit and no one who feels well rehearsed in placing chest tube. General surgeon from Port-au-Prince on his way... It will take 5 hours.
There are more patients who need attention in OR so we need to devise a method to get this patient on to a portable O2. There is one unit with a nasal cannula – Not going to be enough. Ruben and I jerry-rig a face mask with Ambu Bag to patient and unit. Patient brought to recovery.
A word about recovery...
Recovery is a room with NO monitoring equipment. The team has brought three O2 pulseoximeters with us - thank you Ruben. During this process, patients 2 & 3 have been cared for as well.
Ok...so it is 3:30pm now (I regressed a bit) and the one inpatient boy I really wanted to work with (soccer injury), just so happens to wheel himself over to "clinic/PT". I actually had time to work with him and emphasize the importance of working on his own. It will be at least 4 weeks before another PT will be here.
The therapy team meets back on ward to finish up treatment plans, visit with newborn (who I swaddled and gave his first bottle). Mom still unresponsive. We find dad a CHAIR so he can sit down in room. He has not named baby and asks if I would like to name baby. I choose David. They pronounce it Dah-veed, like it is Hebrew.
Also stop by and meet newborn healthy twins with healthy mom. She delivered one day ago. Another teammate was asked to name the twins.
In front of ward there is a courtyard with an unused grassy area. Several team members and translators start up a game of frisbee. It is the first time during the work week where any of us have played around. We attract attention from all of the patients who we have been trying to get outside all week (with great success). Since most of them have some variety of damaged lower extremities, I suggest to the group that we try a “wheel barrel race” and have them race across field while we support their legs (good upper body strengthening!). At first the patients looked at us like we were insane but we talked two into it. Well, this drew just about every staff member and patient out to courtyard to watch. Two of us helped this one patient with a huge fixator devise on his leg. Little did we know that he had a competitive spirit and "walked" so fast on hands, his fixator device practically pierced through my thigh. It was a tie.
So much excitement. Everyone laughing and cheering. More want to race... so this was clearly a highlight of the week as my initial goal was to get everyone outside and create a healthy environment. Said goodbyes to patients and translators after race.
Home for last dinner. Surgeons still in OR. We all head back up to hospital to inquire on surgery cases and recovery room patients. The general surgeon has arrived and the patient with the acute peritonitis (not so acute at this point and surprisingly alive) will finally have his surgery. This is the guy Ruben was running for pain medicine last night when pregnant women showed up. After this surgery patient 1 will get his chest tube. He does not look good. Several team members bring father/husband something to eat. I cannot go back to this room as it is far too emotional for me.
I stop by ER to write/send my initial 48 hour blog (only place with WiFi). Can't write it all at once; too tired and drained.
Final evening, we all debrief about the week and discuss highlights and hard moments. We laugh about some of the crazy stuff that gas happened through out the week. Most of week we had no electricity at house. Hospital operated off generator and would shut down at 10 pm. But lucky for us, we have had electricity since 3:00pm. It is now 1:30 am and I still need to take a cold shower and be up for airport ride at 4:15am... so no sleep for me.
This morning we pack up van, load luggage on top and head out for local airport (75 minutes down the mountain). We are flying to Port-au-Prince as we "weigh a lot less" having unloaded all of our donated goods and can get on a small plane. On way to airport, Sheila gets call from Rudy, the Haitian MD who is in charge (his regular workday schedule is 7:30 am where he leads prayer service to 10:00 pm) I have never seen a doctor work harder with such restricted conditions and manage to still make lots of joked. He has been up all night (second night in a row) and tells Sheila that patient 1 has died and another is being taken back to OR. So much in one week and of course only the tiniest dent on the need in Haiti.
At airport finishing this, looking forward to my husband being at airport and a long HOT shower.
Hard to think about returning to the chaos of our everyday lives. So much to do!!
0 Comments
Last 48 hours: Part Two
March/04/2011 05:48 PM
Friday AM Prayer service
They sing Hatikva in Creole...????
8:00 am: Head to ward.
Baby doing OK.
Mom: no urine output, HTN, heart rate 145. Unconscious
Husband overwhelmed...No one has explained what is going on to dad.
Dealing with mom...when...
Our orthopedic surgeon, Noah, comes to get us...
3 Trauma patients arrived in “ER”:
All morning until 2:30 running around ER and OR. Suddenly I’m a trauma nurse!
There is so much more but I need to go back to house to pack.
I don't think I will ever be the same after this week...
They sing Hatikva in Creole...????
8:00 am: Head to ward.
Baby doing OK.
Mom: no urine output, HTN, heart rate 145. Unconscious
Husband overwhelmed...No one has explained what is going on to dad.
Dealing with mom...when...
Our orthopedic surgeon, Noah, comes to get us...
3 Trauma patients arrived in “ER”:
- Pt. 1: Eyeball out, fractured orbit, head injury, patella fracture, tibia laceration, agitated.
- Pt. 2: Face laceration, huge tibia deep wound, probable head injury
- Pt. 3: Open thigh wound, in shock,
All morning until 2:30 running around ER and OR. Suddenly I’m a trauma nurse!
There is so much more but I need to go back to house to pack.
I don't think I will ever be the same after this week...
Last 48 hours: Part One
March/03/2011 08:00 PM
Thursday night: 8:00 pm rounds in ER
-- Patient with acute peritonitis. No general surgeon.
We leave for ward; our anesthesiologist goes to pharmacy for pain meds.
On ward rounding...
Anesthesiologist comes back — Emergency! Need all of you at ER.
Pregnant woman with eclampsia, seizure at clinic; transferred 2.5 hrs in a FLATBED truck to ER.
She is placed on mat on ground in front of ER, hemorrhaging.
Baby born on mat; mom in distress.
Grab baby with placenta wrapped in someone’s jacket.
Take baby to room; cord cut. No formula. No infant attire
Mom in acute distress, bleeding. O2 65, hypertension 180/130, heart rate 155
Father in shock
Baby; formula; no hot water... also no electricity!
Teammate to guest house; heat water
No GYN, no general surgeon.
Our team stays with pts until 12:30am
Baby fine, but Mom in coma
Dad standing: use a half clean sheet on empty bed for Dad to rest
(patients have to bring all linens, food, etc. - family not prepared)
-- Patient with acute peritonitis. No general surgeon.
We leave for ward; our anesthesiologist goes to pharmacy for pain meds.
On ward rounding...
Anesthesiologist comes back — Emergency! Need all of you at ER.
Pregnant woman with eclampsia, seizure at clinic; transferred 2.5 hrs in a FLATBED truck to ER.
She is placed on mat on ground in front of ER, hemorrhaging.
Baby born on mat; mom in distress.
Grab baby with placenta wrapped in someone’s jacket.
Take baby to room; cord cut. No formula. No infant attire
Mom in acute distress, bleeding. O2 65, hypertension 180/130, heart rate 155
Father in shock
Baby; formula; no hot water... also no electricity!
Teammate to guest house; heat water
No GYN, no general surgeon.
Our team stays with pts until 12:30am
Baby fine, but Mom in coma
Dad standing: use a half clean sheet on empty bed for Dad to rest
(patients have to bring all linens, food, etc. - family not prepared)
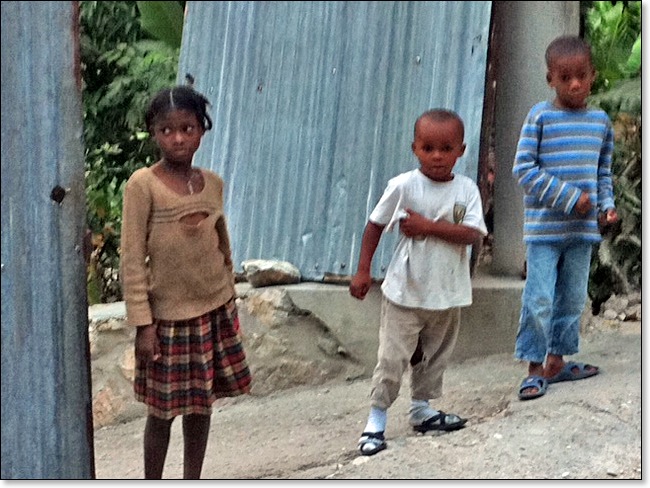
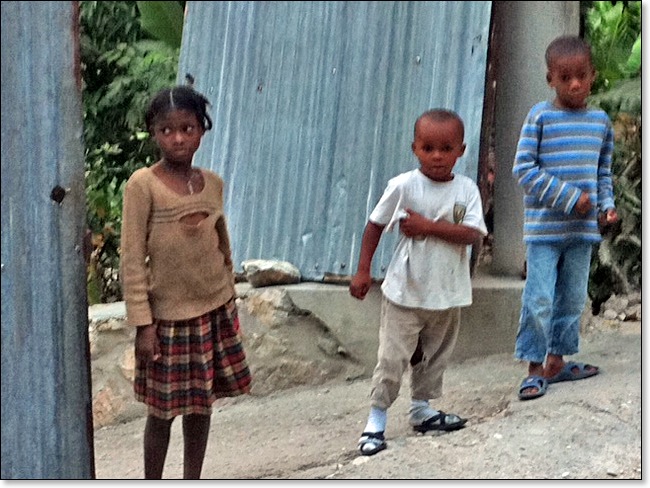
Children who live nearby
March/03/2011 09:33 AM
These children were very excited to see us pass by their home.
Click to view photo location in Google Maps
Click to view photo location in Google Maps
Family leaving funeral
March/02/2011 07:09 PM
A 30-year employee of the hospital died on Monday. The hospital "closed down" this afternoon so staff could attend funeral. I had 2 clinic patients so I missed the service. Funerals are a big deal here. Did catch some good photos after and video.

Click to view photo location in Google Maps
After funeral, 2 guys from hospital took Noah, Ruben, Max and I on a hike to their homes. At Basiwell's home they grow and roast coffee. He wanted us to see his moms hand; carpal tunnel surgery 5 years ago with full hand contracture from not moving it. She may have surgery tomorrow.
On to Jimmy's house. He makes honey and showed us his honeybees. Then he let us taste his honey -- truly fantastic!
The hike provided a real look in to the way the locals live. They have a higher quality of life than Port-au-Prince.
Evening rounds tonight from 7-9:30. Five surgeries scheduled tomorrow; more ortho follow-ups for clinic and 40-50 inpatients who need PT.

Click to view photo location in Google Maps
After funeral, 2 guys from hospital took Noah, Ruben, Max and I on a hike to their homes. At Basiwell's home they grow and roast coffee. He wanted us to see his moms hand; carpal tunnel surgery 5 years ago with full hand contracture from not moving it. She may have surgery tomorrow.
On to Jimmy's house. He makes honey and showed us his honeybees. Then he let us taste his honey -- truly fantastic!
The hike provided a real look in to the way the locals live. They have a higher quality of life than Port-au-Prince.
Evening rounds tonight from 7-9:30. Five surgeries scheduled tomorrow; more ortho follow-ups for clinic and 40-50 inpatients who need PT.
"Haiti Medical Trip February-March 2011"
March/02/2011 06:58 PM
Here is a link to a blog written by the group leader. He is a very kind, helpful and caring man.
http://msreinhard.blogspot.com/
http://msreinhard.blogspot.com/
Little girl/beanie baby
March/01/2011 07:11 AM
Bad picture. The good ones are on regular camera.
This girl's legs were crushed in the earthquake. She has a below knee amp. On right. Her left tibia/fibula have slowly healing fractures. She has a prosthesis for her right which has become the "good leg".
She was sad and serious until I gave her the beanie!!! I am SO glad I brought them.

Click to view photo location in Google Maps
This girl's legs were crushed in the earthquake. She has a below knee amp. On right. Her left tibia/fibula have slowly healing fractures. She has a prosthesis for her right which has become the "good leg".
She was sad and serious until I gave her the beanie!!! I am SO glad I brought them.

Click to view photo location in Google Maps
Day One Ortho clinic, Monday 2/28/11
February/28/2011 07:00 PM
Here is my first full recap of Day One Ortho clinic, Since this recap, I have completed two more days. While the work load is never ending, it is also very fascinating and an experience that I'm glad to be doing. While the group I'm with are very different from me, they are really good people. Hopefully will have more time to write tomorrow. Only 2 more clinic days left.
================================================
Today was the first day of “work”. The tradition is to attend church in the morning at 7:45 and pray with the patients and their families. The music, singing is very moving. They sing from their hearts and the harmony all of the voices in harmony moved me to tears. The Haitians were intrigued by our presence. Many eyes following me across the room. I am the only woman on the trip not “praying” so I stand out a bit. Able to get some video of service to capture the feeling.
Quick rounds/review in the hospital. Families bathing their loved one, cleaning up from the night before; bed mats, sheets on floor, etc. Patients are admitted into the hospital and remain inpatients for reasons that have longed stopped in the US. Clearly no DRGS in Haiti. Examples would include comminuted radius fractures, patella fractures wired together. Then there are the truly complicated patients with multi extremity issues, many of which are old and not healing. Failed ORIF’s, patients with compression syndromes from poor cast placement. Severely fractured pelvis’s being treated with traction pins through the tibia and weights hanging off of the bed. The spirits in the hospital are a little more skeptical. They have been lying in bed feeling ”sick” for a long time. JL’s boot camp will be a shock to the system. My approach: get them up any way they can, ambulate them to outside and treat as many outside as possible to change the environment. The hospital is dark, 8 to a room plus family. Hard to do much at any bedside as a PT; here impossible!!
Off to clinic…The doctors head to the OR and I have an interpreter, Monaville, who will spend the day with me. Let the chaos begin. Complete and utter chaos. There is no system to how cases are triaged and at the same time, the order of patients being seen is not related to first come, first serve…It is far more disorganized and random at the same time. Patients do have to pay for everything being done; X-rays, cortisone shots, medicine, etc. This is not a free clinic. More about that later.
The clinic has two plinths up against the wall with “clean”sheets on each. One has a very firm cushion which is supposed to be the pillow. There is one stool, two chairs which are loaded with things left over from prior clinic days. (x-rays, x-ray frames, “medical records”, etc. The overall feeling put out by the Haitians is hard to describe; a little hopelessness mixed with unrealistic expectations while being detached from their bodies and lacking self initiative to “heal thyself”. I have never had a such a hard time getting people to “move their bodies”. It is not a language barrier. It is the worst body awareness I have ever experienced in any population to date. A BIG PT challenge…
So here is the typical scenario encountered on day one: Patient comes in to clinic with litle to no history written on why they are here. I have to do a full history and ask endless questions trying to get to the reason they chose today to come to ortho clinic. While I am doing this, there is constant interruptions at the door with constant knocking and people wanting to “negotiate” their way to be seen next. Most patients have more than one area of complaint and there is no telling them chose one. So after history and exam, I may have time to actually treat and teach a few things for them to do so unfortunately they miss out on the part of “heal thyself” and thus the pattern continues. I ask over and over again” how important is it to you to get better/full function back? I hear an unconvincing “very important” and try to explain to each patient that he/she will need to endure some pain to get a contractured extremity moving again. I forgot to mention that patients who present with a new problem need x-ray and I write the order for X-ray. Some have had x-ray done before I see them. By the large majority x-rays are over exposed, missing the most important feature you are looking for : label put right over area of issue, over developed right where you need clarity. SO….many need to have x-ray repeated. Clearly the person developing and or shooting the x-ray is not bothering to actually look at developed picture and do a “quality control assessment”. In the states, an ortho would have shot the tech by the third crappy x-ray!
Twenty patients before lunch, I have no idea how. They line to be seen is growing, my interpreter is politely wondering if there will be a break. Little does he know I could work straight through. Bur we do break at 1:15 and agree to return at 2:00. Patients who I have questions about will be seen by the docs at 2:00 before they start a case. Patients are there all day. Part of the helpless mindset.
The afternoon continues much the same as the morning. I have never seen more complicated cases with so many not healing. And at the same time, once again the same surprise exists that what is seen on film and how a patient presents is often shocking. The film would have you believe you have a non ambulating person and yet the patient is somehow managing to walk (with many deficits) on their non healed fractures, pseudoarthrosis, etc.
After a long day; stopped at 6:30, I return to guest house to learn no running water. Okay….After dinner, the lights start to dim and then….no electricity…..Welcome to Haiti! I finish the day taking my cold shower with my “lantern” flashlight (thank god I had it) and go to bed.
================================================
Today was the first day of “work”. The tradition is to attend church in the morning at 7:45 and pray with the patients and their families. The music, singing is very moving. They sing from their hearts and the harmony all of the voices in harmony moved me to tears. The Haitians were intrigued by our presence. Many eyes following me across the room. I am the only woman on the trip not “praying” so I stand out a bit. Able to get some video of service to capture the feeling.
Quick rounds/review in the hospital. Families bathing their loved one, cleaning up from the night before; bed mats, sheets on floor, etc. Patients are admitted into the hospital and remain inpatients for reasons that have longed stopped in the US. Clearly no DRGS in Haiti. Examples would include comminuted radius fractures, patella fractures wired together. Then there are the truly complicated patients with multi extremity issues, many of which are old and not healing. Failed ORIF’s, patients with compression syndromes from poor cast placement. Severely fractured pelvis’s being treated with traction pins through the tibia and weights hanging off of the bed. The spirits in the hospital are a little more skeptical. They have been lying in bed feeling ”sick” for a long time. JL’s boot camp will be a shock to the system. My approach: get them up any way they can, ambulate them to outside and treat as many outside as possible to change the environment. The hospital is dark, 8 to a room plus family. Hard to do much at any bedside as a PT; here impossible!!
Off to clinic…The doctors head to the OR and I have an interpreter, Monaville, who will spend the day with me. Let the chaos begin. Complete and utter chaos. There is no system to how cases are triaged and at the same time, the order of patients being seen is not related to first come, first serve…It is far more disorganized and random at the same time. Patients do have to pay for everything being done; X-rays, cortisone shots, medicine, etc. This is not a free clinic. More about that later.
The clinic has two plinths up against the wall with “clean”sheets on each. One has a very firm cushion which is supposed to be the pillow. There is one stool, two chairs which are loaded with things left over from prior clinic days. (x-rays, x-ray frames, “medical records”, etc. The overall feeling put out by the Haitians is hard to describe; a little hopelessness mixed with unrealistic expectations while being detached from their bodies and lacking self initiative to “heal thyself”. I have never had a such a hard time getting people to “move their bodies”. It is not a language barrier. It is the worst body awareness I have ever experienced in any population to date. A BIG PT challenge…
So here is the typical scenario encountered on day one: Patient comes in to clinic with litle to no history written on why they are here. I have to do a full history and ask endless questions trying to get to the reason they chose today to come to ortho clinic. While I am doing this, there is constant interruptions at the door with constant knocking and people wanting to “negotiate” their way to be seen next. Most patients have more than one area of complaint and there is no telling them chose one. So after history and exam, I may have time to actually treat and teach a few things for them to do so unfortunately they miss out on the part of “heal thyself” and thus the pattern continues. I ask over and over again” how important is it to you to get better/full function back? I hear an unconvincing “very important” and try to explain to each patient that he/she will need to endure some pain to get a contractured extremity moving again. I forgot to mention that patients who present with a new problem need x-ray and I write the order for X-ray. Some have had x-ray done before I see them. By the large majority x-rays are over exposed, missing the most important feature you are looking for : label put right over area of issue, over developed right where you need clarity. SO….many need to have x-ray repeated. Clearly the person developing and or shooting the x-ray is not bothering to actually look at developed picture and do a “quality control assessment”. In the states, an ortho would have shot the tech by the third crappy x-ray!
Twenty patients before lunch, I have no idea how. They line to be seen is growing, my interpreter is politely wondering if there will be a break. Little does he know I could work straight through. Bur we do break at 1:15 and agree to return at 2:00. Patients who I have questions about will be seen by the docs at 2:00 before they start a case. Patients are there all day. Part of the helpless mindset.
The afternoon continues much the same as the morning. I have never seen more complicated cases with so many not healing. And at the same time, once again the same surprise exists that what is seen on film and how a patient presents is often shocking. The film would have you believe you have a non ambulating person and yet the patient is somehow managing to walk (with many deficits) on their non healed fractures, pseudoarthrosis, etc.
After a long day; stopped at 6:30, I return to guest house to learn no running water. Okay….After dinner, the lights start to dim and then….no electricity…..Welcome to Haiti! I finish the day taking my cold shower with my “lantern” flashlight (thank god I had it) and go to bed.
Little girl sleeping on floor
February/27/2011 07:15 PM
This little girl sleeps on the floor of the hospital keeping her dad company. Bad picture, beautiful little girl. Just finished evening rounds. Tomorrow we have around 30 inpatients needing PT. They are expecting 20 outpatients tomorrow who are post op follow up earthquake victims. I have been asked to do all screening as docs are in OR.
I have 4 people working under me (pTA's and OT). Should be a busy day.
Hope to sleep better tonight; last night rooster crowed ALL night. Then the two dogs got in to a fight with the rooster around 3:00am......

Click to view photo location in Google Maps
I have 4 people working under me (pTA's and OT). Should be a busy day.
Hope to sleep better tonight; last night rooster crowed ALL night. Then the two dogs got in to a fight with the rooster around 3:00am......

Click to view photo location in Google Maps
Haiti first impressions
February/27/2011 07:01 AM
We arrived and got through customs quickly - not much concern for what you are bringing in here. Once outside (hot, humid, 80's, I'm loving it), the haggling begins. Forty to fifty men trying to get you to use their vehicle. We had a prearranged van for all 10 of us. Luggage on top strapped down. The chain link fence separating Haiti from the airport has young boys begging you to give them money. Once outside the airport the rule of the road is the bigger the car and the louder the horn ==> the right of way. Horns are used like doorbells to announce your presence. Constant honking the whole way. A few streets away from the airport we were in a congested area. Lots of people on streets, many approaching the van. One person in our van saw the shadow of a person up on top of our van, pulling at the ropes. We all got a little concerned...ok very concerned. The bus driver then explained we had a hired person on top of van "to keep luggage tied". That was a HUGE relief.
As you ride through Port-au-Prince there is no sign that things have been cleaned up other than the streets are cleared, mostly. Building after building toppled and tents set up around the rubble. People live literally on top of one another. Existing structures are attached, 6x6' and stack up from street back to who knows where. So before earthquake, the people living in this area were already living on top of one another. No privacy. Areas with tent camps have the tents attached to one another... Again, 6x6, stacked together.
What did catch my eye is the interesting tin used for entry ways and garage doors. The kind of tin with imprints that I would like to arrange to ship home and use somewhere in my 9x9 house! The tin and iron grates are decorative.
What's most decorative are the tap tap buses. Painted, decorated, usually religiously themed but not always. The owners of the buses compete with design to be the best tap tap bus. This guarantees more ridership. People pile on, and I mean pile. The highlight was catching up to the Barack Obama tap tap bus. My favorite!
The damage from the earthquake was visible through the first 90 minutes of our ride. Now we weren't driving fast but even still, the damage was far-reaching.
At one point we started driving through the country, very lush, reminds me of Costa Rica. Every few miles you ride in to a little bazaar with street side vendors. I could not convince them to let me out and look around for hidden treasures. Dogs run along the road and cars/buses honk at them. That's the only warning they get so unfortunately I got to see the tap tap bus ahead of us hit a dog and kill it.........
We drove to the southwest area of the island called Calles. We were met by the group leader Sheila. The van would never make it up the steep winding road to hospital.
Everyone out, loaded luggage in to jeep, and all but me climbed on TOP of jeep to ride up the mountain. I rode in jeep next to Sheila. She has lived here for almost 3 years. I really like her spirit. That’s me behind the jeep in the photo below.

The guest house is quite livable. Five bedrooms, 3 baths sometimes with running water (cold). We have two house staff who cooked a great dinner. I passed on the goat but otherwise liked the rice, beans, cole slaw, tomatoes, chicken, plantain and coconut cookie.

After dinner we went to hospital to round on all 50 patients and a few in ER. Rooms have 6-8 patients plus family. It is not unusual for a family member to sleep under the bed of a loved one to care for them.
Wow diabetes – not the American variety from poor diet and obesity. These people are thin. Diabetic ulcers that don't heal and after several failed attempts to debride, end up with amputations. All ages, men and woman.
Trauma fractures from vehicle accidents. Motorcycle (the no helmet varieties) with head trauma as an added bonus. Lots of badly displaced fractures, some open through the skin. Pins, plates, bone traction with weights hanging off bed. BEDREST for 4 plus weeks. A PT nightmare. No get em up and move them day 1. Severe deconditioning, atrophy, and yes, decubiti... more bad healing. Every patient here has been referred to me to design a program. Noah will be doing some tendon releases to free up contractures caused by immobility. The patients are comfortable for the most part. Not a lot of pain meds here. Lots of smiles. One boy here for a displaced tibia fracture from a bad soccer play, is adorable. He will have surgery Monday to fixate his fracture and then he's all mine. Most like my current population!!!
The hardest case was a young girl 2-3, with a fractured radius. Taken to an herbalist who wrapped her arm too tight and resulted in a compartment syndrome. She is in pain. Huge tears and crying when her bandages were removed...and she cried too. Big tears, fear in her eyes, screaming from pain. Surgery for her. Many beanie babies and toys are coming to her. She is beautiful.... and her mother very present.
On walk back to house, I spotted a beautiful toad/frog... I knew Eric was with me!!! Others went to look for tarantulas in the rocks. I passed on that...
All for now.....
As you ride through Port-au-Prince there is no sign that things have been cleaned up other than the streets are cleared, mostly. Building after building toppled and tents set up around the rubble. People live literally on top of one another. Existing structures are attached, 6x6' and stack up from street back to who knows where. So before earthquake, the people living in this area were already living on top of one another. No privacy. Areas with tent camps have the tents attached to one another... Again, 6x6, stacked together.
What did catch my eye is the interesting tin used for entry ways and garage doors. The kind of tin with imprints that I would like to arrange to ship home and use somewhere in my 9x9 house! The tin and iron grates are decorative.
What's most decorative are the tap tap buses. Painted, decorated, usually religiously themed but not always. The owners of the buses compete with design to be the best tap tap bus. This guarantees more ridership. People pile on, and I mean pile. The highlight was catching up to the Barack Obama tap tap bus. My favorite!
The damage from the earthquake was visible through the first 90 minutes of our ride. Now we weren't driving fast but even still, the damage was far-reaching.
At one point we started driving through the country, very lush, reminds me of Costa Rica. Every few miles you ride in to a little bazaar with street side vendors. I could not convince them to let me out and look around for hidden treasures. Dogs run along the road and cars/buses honk at them. That's the only warning they get so unfortunately I got to see the tap tap bus ahead of us hit a dog and kill it.........
We drove to the southwest area of the island called Calles. We were met by the group leader Sheila. The van would never make it up the steep winding road to hospital.
Everyone out, loaded luggage in to jeep, and all but me climbed on TOP of jeep to ride up the mountain. I rode in jeep next to Sheila. She has lived here for almost 3 years. I really like her spirit. That’s me behind the jeep in the photo below.

The guest house is quite livable. Five bedrooms, 3 baths sometimes with running water (cold). We have two house staff who cooked a great dinner. I passed on the goat but otherwise liked the rice, beans, cole slaw, tomatoes, chicken, plantain and coconut cookie.

After dinner we went to hospital to round on all 50 patients and a few in ER. Rooms have 6-8 patients plus family. It is not unusual for a family member to sleep under the bed of a loved one to care for them.
Wow diabetes – not the American variety from poor diet and obesity. These people are thin. Diabetic ulcers that don't heal and after several failed attempts to debride, end up with amputations. All ages, men and woman.
Trauma fractures from vehicle accidents. Motorcycle (the no helmet varieties) with head trauma as an added bonus. Lots of badly displaced fractures, some open through the skin. Pins, plates, bone traction with weights hanging off bed. BEDREST for 4 plus weeks. A PT nightmare. No get em up and move them day 1. Severe deconditioning, atrophy, and yes, decubiti... more bad healing. Every patient here has been referred to me to design a program. Noah will be doing some tendon releases to free up contractures caused by immobility. The patients are comfortable for the most part. Not a lot of pain meds here. Lots of smiles. One boy here for a displaced tibia fracture from a bad soccer play, is adorable. He will have surgery Monday to fixate his fracture and then he's all mine. Most like my current population!!!
The hardest case was a young girl 2-3, with a fractured radius. Taken to an herbalist who wrapped her arm too tight and resulted in a compartment syndrome. She is in pain. Huge tears and crying when her bandages were removed...and she cried too. Big tears, fear in her eyes, screaming from pain. Surgery for her. Many beanie babies and toys are coming to her. She is beautiful.... and her mother very present.
On walk back to house, I spotted a beautiful toad/frog... I knew Eric was with me!!! Others went to look for tarantulas in the rocks. I passed on that...
All for now.....
Arrived in Haiti
February/26/2011 07:51 PM
So much to take in. The devastation and how people are living right around it, on it, over it... Took about 6 hours to get to hospital. The ride was a very interesting experience.
The hospital has 50 patients needing various surgeries related to diabetic ulcers needing amputations, trauma fractures, a few earthquake follow-ups procedures for failed cases.
Many, many stories already. The CA gang is great...
The hospital has 50 patients needing various surgeries related to diabetic ulcers needing amputations, trauma fractures, a few earthquake follow-ups procedures for failed cases.
Many, many stories already. The CA gang is great...

